Table of Contents
Click here to download the Practice Guidance as a pdf
These guidelines were developed by a Task and Finish group, working on behalf of the Cambridgeshire and Peterborough Safeguarding Adults Board, and were adopted by the SAB in July 2019.
Membership of the group included:
- CPFT (TVN, Neighbourhood Team Nurses, Safe Guarding Lead, MDT Co Coordinator)
- Social Care: Cambs County Council, Cambs MASH
- Papworth (TVN)
- CCG (Lead Nurse for Care Homes, Safe Guarding)
- SAB
- NWAFT (TVN)
- Care Homes
The following guidelines were written to support the Pressure Ulcer Protocol Published by Department of Health & Social Care in January 2018, and aim to assist practitioners understand the interface between the protocol and a safeguarding enquiry.
What is a pressure ulcer?
A pressure ulcer is an area of damage to the skin and underlying tissue. They are sometimes known as pressure sores or bed sores.
What causes a pressure ulcer?
Pressure ulcers are caused by poor circulation to tissues due to a combination of the following factors:
- Pressure – Body weight and some equipment (e.g. anti-thrombosis stockings) can squash the skin and other tissues where parts are under pressure. This reduces the blood supply to the area and can lead to tissue damage.
- Shearing – Sliding or slumping down the bed/chair can damage the skin and deeper layers of tissue.
- Friction – Poor moving and handling methods can remove the top layers of skin. Repeated friction can increase your risk.
Who is most at risk of developing pressure ulcer?
You may be at risk of developing pressure ulcers for a number of reasons including the following:
- Problems with movement – If your ability to move is limited and you are unable to change position regularly or are in a wheel chair.
- Poor circulation – Vascular disease or smoking reduces your circulation.
- Moist skin – You may be at increased risk if your skin is too damp.
- Lack of sensitivity to pain or discomfort – Conditions such as diabetes, stroke, nerve/muscle disorders reduce the normal sensations that usually prompt you, or enable you to move. Some treatments (e.g. epidural pain relief, medication, operations) reduce your sensitivity to pain or discomfort so that you are not aware of the need to move.
- Previous tissue damage – Scar tissue will have lost some of its previous strength and is more prone to breakdown.
- Inadequate diet or fluid intake – Lack of fluid may dehydrate your tissues. Weight gain or loss can affect the pressure distribution over bony points and healing.
- People having problems with memory – and understanding who may not be able to follow advice and guidance.
Risk Assessment
To assess your risk of developing pressure ulcers, a member of your health care team will examine/asses you and ask you some questions. This will help to identify if you require any specialised equipment or other forms of care, and will assist in providing for your individual needs.
What are the early signs of a pressure ulcer?
You will notice the following signs:
- Change in skin colour, redder or darker
- Heat or cold
- Discomfort or pain
- Blistering, swelling
- Skin damage
Without appropriate intervention the damage may worsen, developing into hard black tissue or an open wound.
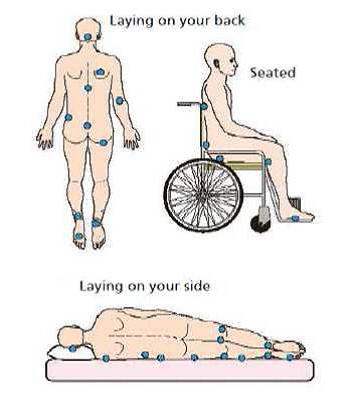
Common locations of pressure ulcers
What can I do to avoid pressure ulcers?
There are several ways you can reduce the risk of pressure ulcers.
- Keep moving – Changing your position regularly helps keep blood flowing. If you have reduced movement the health care team looking after you will assist you with regular turns in addition to providing specialist mattresses, cushions and other equipment.
- Look for signs of damage – Check your skin for pressure damage at least once a day. Look for skin that doesn’t go back to its normal colour after you have taken your weight off it. Do not continue to lie on skin that is redder or darker than usual. Also watch out for blisters, dry patches or breaks in the skin.
- Protect your skin – Wash your skin using warm water and non-perfumed soap. If you suffer from incontinence please inform your health care team as they can assess the best way to deal with your problems. Rubbing/massaging using a ring cushion is not recommended.
- Eat a well-balanced diet – Make sure you eat a healthy balanced diet and drink plenty of fluids. Extra protein may help.
What should I do if I suspect a pressure ulcer?
Tell your doctor or nurse as soon as possible and follow the advice they give you.
Pressure Ulcers can be a safeguarding concern. This is more likely where the ulcer is avoidable and serious in its impact. They are frequently associated with other safeguarding concerns, such as neglect and self-neglect. These can include poor diet, inadequate care and inappropriate physical handling. Pressure Ulcers can be the result of appropriate equipment not being accepted or used, which could be Domestic Abuse.
It is vital that any consideration of Pressure Ulcers being linked to safeguarding includes a wider consideration of whether other concerns over abuse and/or neglect are present for the Adult at Risk.
Professional and medical information on the identification, assessment and treatment of Pressure Ulcers can be found at:
Information for the wider public is available at https://www.nice.org.uk/guidance/cg179/ifp/chapter/What-is-a-pressure-ulcer
Local resources
CPFT provide District Nursing Services for Cambridgeshire and Peterborough. For smaller providers without Tissue Viability Nurses then advice should be sought from the GP or, if they have one, the adult’s District Nurse. Resources and guidance is available on CPFT’s website at https://www.cpft.nhs.uk/search-results.htm?sitekit=true&task=search&indexname=Site&blah=&search=PRESSUE+ULCERS
https://improvement.nhs.uk/resources/Using-SSKIN-to-manage-and-prevent-pressure-damage/
Safeguarding
To assist in deciding whether an ulcer should be considered a safeguarding concern, there is a national Safeguarding Protocol that can be found at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/675192/CSW_ulcer_protocol_guidance.pdf
FLOW CHART
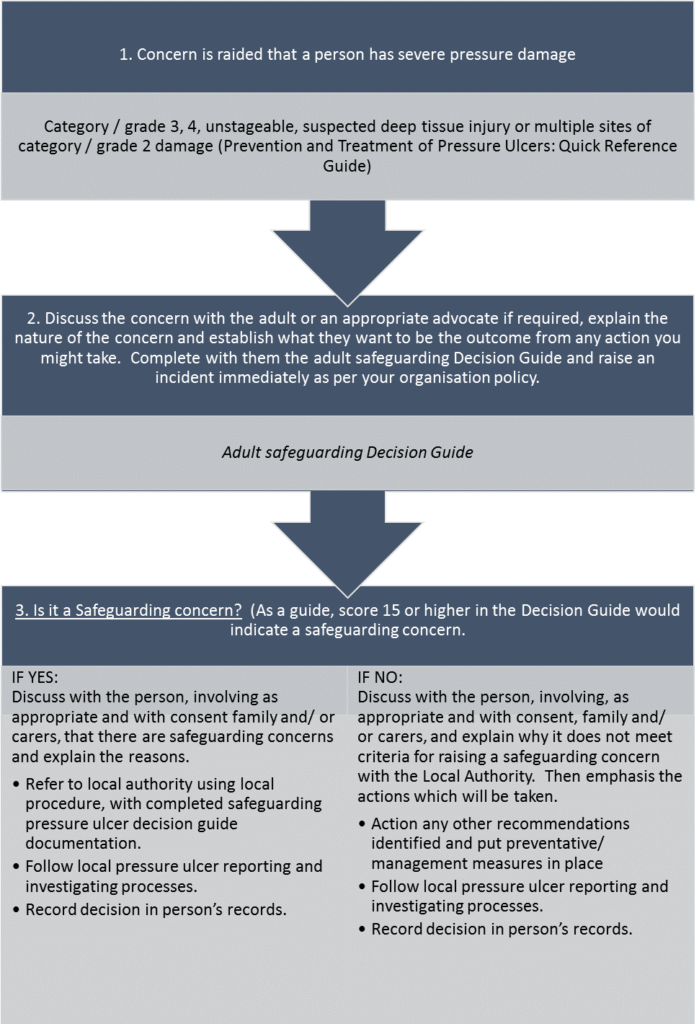
Adult Safeguarding Decision Guide for individuals with severe pressure ulcers
Adult Safeguarding Decision Guide for Individuals with severe pressure ulcers
[1] Reference: Whiting NL (2009) Skin assessment of patients at risk of pressure ulcers. Nursing Standard vol 24 no. 10 pages 40 – 44
