Table of Contents
RELATED GUIDANCE
- Sex and Relationships Education (SRE) For The 21st Century
- Statutory guidance on relationships education, relationships and sex education (RSE) and health education.
- SRE – The Evidence (Sex Education Forum publication, March 2015)
1. Flowchart for Professionals Working With Sexually Active Under 18’s
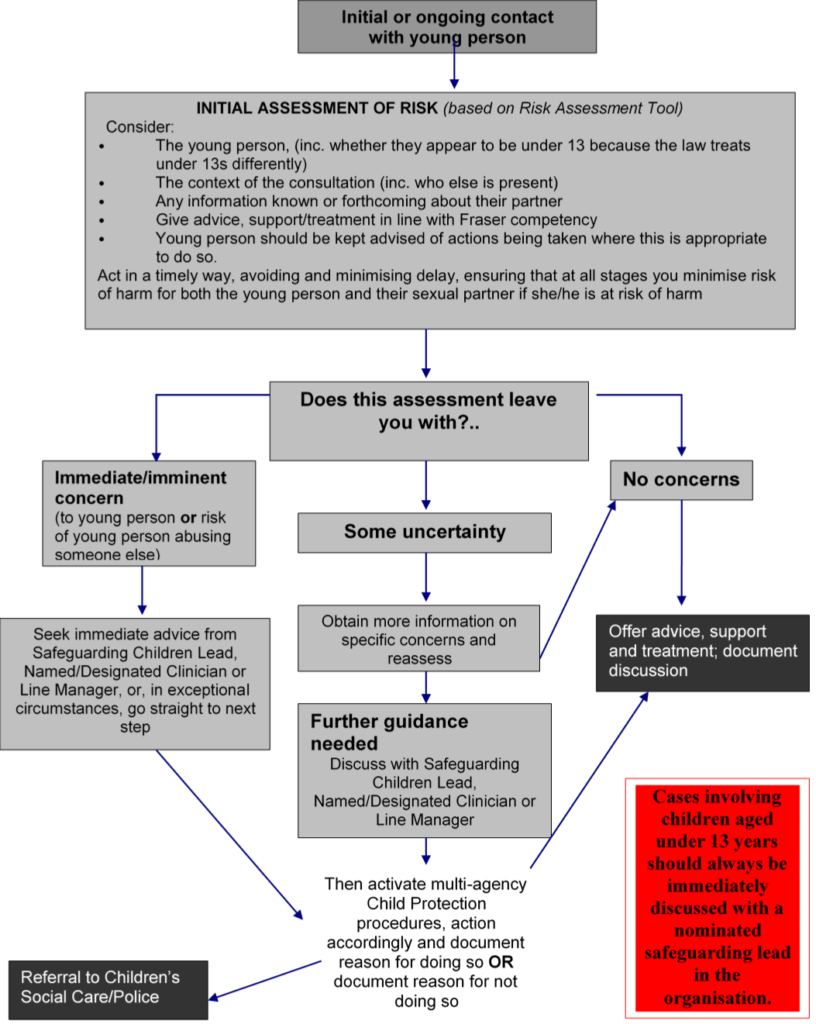
Click here to view the Flowchart for Professionals Working With Sexually Active Under 18’s.
2. Introduction
This guidance has been devised with the understanding that most young people under the age of 18 will have an interest in sex and sexual relationships.
It is designed to assist those working with children and young people to identify where these relationships may be abusive, and where the children and young people may need protection or additional services.
It is based on the core principle that the welfare of the child or young person is paramount, and it emphasises the need for professionals to work together in accurately assessing the likelihood of Significant Harm when a child or young person is engaged in sexual activity.
3. Assessment
All young people under the age of 16 who are believed to be engaged in, or planning to be engaged in, sexual activity should have their needs for health education, support and/or protection assessed by the agency involved. Where possible this assessment should be carried out using the Risk Assessment Tool (see Appendix 3: Safeguarding Children Board Risk Assessment Tool) and in accordance with:
- Peterborough and Cambridgeshire Safeguarding Children Board’s Procedures;
- Department of Health Best Practice Guidance for Doctors and other Health Professionals on the provision of advice and treatment to young people under 16 on contraception, sexual and reproductive health (see Appendix 2: DOH Best Practice Guidance for Doctors and other Health Professionals (DoH 2004)).
3.1 Child Sexual Exploitation (CSE)
In assessing the nature of any relationship and whether the relationship is exploitative or presents a risk to the young person, the following factors should be considered. This list is not exhaustive and other factors may need to be taken into account:
- Whether the young person is competent to understand and consent to the sexual activity he/she is involved in;
- The nature of the relationship between those involved, particularly if there are age or power imbalances as outlined below;
- Whether overt aggression, coercion or bribery was involved including misuse of substances/alcohol as a disinhibitor;
- Whether the young person’s own behaviour, for example through misuse of substances, including alcohol, places him/her in a position where he/she is unable to make an informed choice about the activity;
- Any attempts to secure secrecy by the sexual partner beyond what would be considered usual in a teenage relationship;
- Whether the sexual partner is known by the agency as having other concerning relationships with similar young people;
- If accompanied by an adult, does that relationship give you any cause for concern?
- Whether the young person denies, minimises or accepts concerns;
- Whether methods used to secure compliance and/or secrecy by the sexual partner are consistent with behaviours considered to be grooming (See Appendix 1: Additional Information);
- Whether sex has been used to gain favours (e.g. swap sex for cigarettes, clothes, CDs, trainers, alcohol, drugs etc);
- The young person has a lot of money or other valuable things, which cannot be accounted for.
Concerns identified from this list are indicators that a child is at risk of or experiencing sexual exploitation and professionals should seek advice immediately from their safeguarding lead, as well as referring concerns to Children’s Social Care using the form and CSE checklist.
3.2 Young People with Disabilities
If the young person has a learning disability, additional or complex needs, mental disorder or other communication difficulty, they may not be able to communicate easily to someone that they are, or have been abused, or subjected to abusive behaviour. Staff need to be aware that the Sexual Offences Act 2003 (See Appendix 1: Additional Information) recognises the rights of people with a mental disorder to a full life, including a sexual life. However, there is a duty to protect them from abuse and exploitation and it is of particular importance to ensure that the matter of consent is considered with young people who may have a learning difficulty or disability (see Appendix 1: Additional Information). They are likely to be considered as children in need too
3.3 Fraser Guidelines
It is considered good practice for workers to follow the Fraser guidelines when discussing personal or sexual matters with a young person under 16. The Fraser guidelines give guidance on providing advice and treatment to young people under 16 years of age. These assert that sexual health services can be offered without parental consent providing that:
- The young person understands the advice that is being given;
- The health professional cannot persuade the young person to inform his/her parents or allow the doctor to inform the parents that he/she is seeking contraceptive advice;
- The young person is likely to begin or continue to have sexual intercourse with or without contraceptive treatment;
- The young person’s physical or mental health is likely to suffer unless he/she receives contraceptive advice or treatment;
- It is in the young person’s best interests to receive contraception/safe sex advice and treatment without parental consent.
4. Process
4.1 Confidentiality
In working with young people, it must always be made clear to them that absolute confidentiality cannot be guaranteed, and that there will be some circumstances where the needs of the young person can only be safeguarded by sharing information with others.
This discussion with the young person may prove useful as a means of emphasising the gravity of some situations.
4.2 Assessment of risk and sexual exploitation
On each occasion that a young person is seen by an agency, the Risk Assessment must be completed or updated. Then consideration should be given as to whether their circumstances have changed or further information has been given which may lead to the need for referral or re-referral.
In some cases urgent action may need to be taken to safeguard the welfare of the young person, for example if it is suspected that they are at risk of sexual exploitation. In these circumstances, there must be an immediate referral to Referral Centre or Out of hours Emergency Duty team (Children’s Social Care) or the Police Central Referral Unit (see Report a Safeguarding Concern). In most circumstances there will need to be a process of information sharing and discussion in order to formulate an appropriate plan. There should be time for reasoned consideration to define the best way forward.
Anyone concerned about the sexual activity of a young person must initially discuss this with the person in their agency responsible for safeguarding children. There may be the need for a further consultation with Referral Centre or out of hours Emergency Duty team (Children’s Social Care) or the Police Central Referral Unit. In many cases, it will not be in the best interests of the young person for criminal or civil proceedings to be instigated. However, police and Children’s Social Care and other agencies may hold vital information that will assist in any clear assessment of risk.
All discussions should be recorded, giving reasons for action taken and who was spoken to.
It is important that all decision making, regarding concerns, is undertaken with full professional consultation, never by one person alone.
4.3 Referrals
If you have concerns that the young person may be at risk of sexual exploitation, please refer to Children’s Social Care.
The referral will be triaged by the MASH (Multi Agency Safeguarding Hub) where a possible case discussion/strategy meeting will take place.
Please see following responses:
- No further action deemed necessary;
- An Initial Assessment undertaken which may identify the young person as a ‘Child in Need‘ and additional services provided;
- An Initial Assessment undertaken which may identify the young person as a child at risk of Significant Harm and a Section 47 Enquiry is undertaken.
Following any referral to Children’s Social Care and after a Strategy Discussion with the Police and/or other agencies there may be one of these responses:
- No further action deemed necessary;
- An Initial Assessment undertaken which may identify the young person as a ‘Child in Need’ and additional services provided;
- An Initial Assessment undertaken which may identify the young person as a child at risk of Significant Harm and a Section 47 Enquiry is undertaken.
The outcome of the referral will be formally fed back to the referring agency and during this process agencies must continue to offer the service and support to the young person.
4.4 Escalation
‘It is the responsibility of all professionals to present a challenge to the actions and decisions of other agencies where they believe they have evidence to suggest that the child’s development or safety may be compromised.’ For further advice and guidance see the Resolving Professional Differences (Escalation) Policy.
4.5 Pregnancy
Any girl under the age of 16, who is pregnant, must be offered specialist support and guidance by the relevant services. Any child protection concerns must be discussed with the safeguarding children lead.
When a girl under 13 is found to be pregnant, a referral to Children’s Social Care must be made and the relevant action will be taken.
5. Young People Under the Age of 13
Under the Sexual Offences Act 2003, children under the age of 13 are considered of insufficient age to give consent to any form of sexual activity. Therefore penetrative sex with a child under the age of 13 is classed as rape.
In all cases where the sexually active young person is under the age of 13, a full risk assessment must be undertaken using the Risk Assessment Tool (see Appendix 3: Safeguarding Children Board Risk Assessment Tool). Each case MUST be discussed with the Safeguarding lead and a referral MUST be made to Referral and Assessment (Children’s Social Care) and Police Central Referral Unit. In order for this to be meaningful, the young person will need to be identified, as will their sexual partner if details are known.
A Strategy discussion/meeting will be held and the SARC Mountain Healthcare sexual health screening pathway for under 13years will be followed.
6. Young People between 13 and 15
The Sexual Offences Act 2003 reinforces that, although mutually agreed, non-exploitative sexual activity between teenagers does take place and that often no harm comes from it, the age of consent should still remain at 16. This acknowledges that this group of young people are still vulnerable, even when they do not view themselves as such.
Sexually active young people in this age group must be assessed using the Risk Assessment Tool (see Appendix 3: Safeguarding Children Board Risk Assessment Tool). Discussion with the safeguarding lead will depend on the level of risk/need assessed by those working with the young person.
This difference in procedure reflects the position that, whilst sexual activity under 16 remains illegal, young people under the age of 13 are not deemed legally capable to give consent to such sexual activity.
Consent should be fully explored with this age group to ensure the young person had both the capacity and choice to engage in sexual activity – the absence of either demonstrates a risk of significant harm through abuse or sexual exploitation.
7. Young People Between 16-17
Although sexual activity in itself is not an offence over the age of 16, young people under the age of 18 are still offered the protection of multi-agency safeguarding children procedures under the Children’s Act 2004. Consideration still needs to be given to issues of child sexual exploitation and whether consent was understood and given to sexual activity by the young person.
Young people, of course, can still be subject to offences of rape and assault and the circumstances of an incident may need to be explored with a young person. Young people over the age of 16 and under the age of 18 are not deemed able to give consent if the sexual activity is with an adult in a position of trust or a family member as defined in the Sexual Offences Act 2003.
See Appendix 6: Consent – Cup of Tea.
8. Sharing Information with Parents and Carers
Decisions to share information with parents and carers will be taken using professional judgement, consideration of Fraser guidelines and in consultation with the Child Protection Procedures. Decisions will be based on the child’s age, maturity and ability to appreciate implications and risks to themselves. This should be coupled with the parents’ and carers’ ability and commitment to protect the young person. Given the responsibility that parents have for the conduct and welfare of their children, professionals should encourage the young person, to share the information with their parents and carers wherever safe to do so.
All decisions must be clearly documented on the Risk Assessment and child’s records.
This guidance is written on the understanding that those working with this vulnerable group of young people will naturally want to do as much as they can to provide a safe, accessible and confidential service whilst remaining aware of their duty of care to safeguard them and promote their well-being.
It is intended that this guidance will be reviewed in accordance with Peterborough and Cambridgeshire Safeguarding Children’s Board’s requirements or following changes in legislation and/or change in national guidance.
Appendix 1: Additional Information
Definitions
Sexual Grooming
Section 15 of the Sexual Offences Act 2003 makes it an offence for a person (A) aged 18 or over to meet intentionally, or to travel with the intention of meeting a child under 16 in any part of the world, if he/she has met or communicated with that child on one or more occasions, and intends to commit a “relevant offence” against that child either at the time of the meeting or on a subsequent occasion. An offence is not committed if (A) reasonably believes the child to be 16 or over.
Child Sexual Exploitation
Child sexual exploitation is a form of child sexual abuse. It occurs where an individual or group takes advantage of an imbalance of power to coerce, manipulate or deceive a child or young person under the age of 18 into sexual activity (a) in exchange for something the victim needs or wants, and/or (b) for the financial advantage or increased status of the perpetrator or facilitator. The victim may have been sexually exploited even if the sexual activity appears consensual. Child sexual exploitation does not always involve physical contact; it can also occur through the use of technology.
The Sexual Offences Act 2003
The Age of Consent
The legal age for young people to consent to have sex is still 16, whether they are straight, gay or bisexual. The aim of the law is to protect the rights and interests of young people, and make it easier to prosecute people who pressure or force others into having sex they don’t want.
For the purposes of the under 13 offences, whether the child consented to the relevant risk is irrelevant. A child under 13 does not, under any circumstances, have the legal capacity to consent to any form of sexual activity.
Definition of Consent within Sexual Offences Act 2003
Section 74 defines consent: ‘a person consents if he agrees by choice, and has the freedom and capacity to make that choice‘.
This definition should be considered in two stages. They are:
- Whether a complainant had the capacity (i.e. the age and understanding) to make a choice about whether or not to take part in the sexual activity at the time in question;
- Whether he or she was in a position to make that choice freely, and was not constrained in any way. Assuming that the complainant had both the freedom and capacity to consent, the crucial question is whether the complainant agrees to the activity by choice.
The question of capacity to consent is particularly relevant when a complainant is intoxicated by alcohol or affected by drugs.
See Crown Prosecution Service website.
Protecting people with a mental disorder
The act has created three new categories of offences to provide additional protection with a mental disorder:
- The Act covers offences committed against those who, because of a profound mental disorder, lack the capacity to consent to sexual activity;
- The Act covers offences where a person with a mental disorder is induced, threatened or deceived into sexual activity;
- The Act makes it an offence for people providing care, assistance or services to someone in connection with a mental disorder to engage in sexual activity with that person.
Children and Families: Safer From Sexual Crime – (The Sexual Offences Act 2003)
Although the age of consent remains at 16, the law is not intended to prosecute mutually agreed teenage sexual activity between two young people of a similar age, unless it involves abuse or exploitation. Young people, including those under 13, will continue to have the right to confidential advice on contraception, condoms, pregnancy and abortion.
Allegations of harm arising from underage sexual activity
Cases involving children aged under 13 years should always be discussed with a nominated safeguarding lead in the organisation. Under the Sexual Offences Act, penetrative sex with a child under 13 years old is classed as rape. Where the allegation concerns penetrative sex, or other intimate sexual activity occurs, there would always be reasonable cause to suspect that a child, whether girl or boy, is suffering, or is likely to suffer, significant harm. There should be a presumption that the case will be reported to children’s social care and that a strategy discussion will be held. This should involve children’s social care, police, health and other relevant agencies in discussing appropriate next steps with the professional. All cases involving under 13s should be fully documented including detailed reasons where a decision is taken not to share information. These decisions should be exceptional and only made with the documented approval of a senior manager.
Additional References
Enabling young people to access contraceptive and sexual health information and advice: Legal and Policy Framework for Social Workers, Residential Social Workers, Foster Carers and other Social Care Practitioners.
(Department for Education and Skills Teenage Pregnancy Unit 2004)
Best practice guidance for doctors and health professionals on the provision of advice and treatment to young people under 16 on contraception, sexual and reproductive health.
(Department of Health July 2004)
What to do if you are worried a child is being abused; Children’s Services Guidance.
(Joint publication from the Department of Health, Home Office, Office of the Deputy Prime Minister, Lord Chancellor, Department of Education and Skills).
Further Information Available From:
Appendix 2: DOH Best Practice Guidance for Doctors and other Health Professionals (DoH 2004)
Summary
This revised guidance replaces HC (86)1/HC (FP) (86)1/LAC (86)3 which is now cancelled. Doctors and health professionals have a duty of care and a duty of confidentiality to all patients, including under 16s.
This guidance applies to the provision of advice and treatment on contraception, sexual and reproductive health, including abortion.
Nearly a third of men and a quarter of women aged 16–19 had heterosexual intercourse before they were 16. The UK continue to have the highest teenage birth and abortion rates in Western Europe.
In England in 2013 there were 22,830 under 18 conceptions. A rate of 24.3 per 1000 females aged 15-17. More than half (51.5 per cent) of the pregnancies were terminated. In Cambridgeshire in 2013 there were 173 conceptions in young people age under 18, a rate of 16.1 (down from 31.4 in 1998) per 1000 females aged 15-17.
Avery L and Lazdane G, What do we know about sexual and reproductive health of adolescents in Europe? European Journal of Contraception and Reproductive Health Care vol 13, no 1, March (2008) pp 58-70.
Young people under 16 are the group least likely to use contraception and concern about confidentiality remains the biggest deterrent to seeking advice. Publicity about the right to confidentiality is an essential element of an effective contraception and sexual health service.
Action
- Clinical commissioners and clinical governance leads should bring this guidance to the attention of all health professionals responsible for the care of young people in any setting. All services providing contraceptive advice and treatment to young people should:
- Produce an explicit confidentiality policy making clear that under 16s have the same right to confidentiality as adults;
- Prominently advertise services as confidential for young people under 16, within the service and in community settings where young people meet.
- Health professionals who do not offer contraceptive services to under 16s see that there are arrangements in place for them to be seen elsewhere urgently;
- Directors of Children’s Services should ensure that social care professionals working with young people are aware of this guidance and the Teenage Pregnancy Unit Guidance (2004) ‘Enabling young people to access contraception and sexual health information and advice: the legal and policy framework for social workers, foster carers and other social care practitioners’.
Confidentiality
The duty of confidentiality owed to a person under 16, in any setting, is the same as that owed to any other person. This is enshrined in professional codes.
All services providing advice and treatment on contraception, sexual and reproductive health should produce an explicit confidentiality policy, which reflects this guidance and makes clear that young people under 16 have the same right to confidentiality as adults.
Confidentiality policies should be prominently advertised, in partnership with health, education, youth and community services. Designated staff should be trained to answer questions. Local arrangements should provide for people whose first language is not English or who have communication difficulties.
Employers have a duty to ensure that all staff maintains confidentiality, including the patient’s registration and attendance at a service. They should also organise effective training, which will help fulfil information governance requirements.
Confidentiality: protecting and providing information
General Medical Council, London. (2009) Code of professional conduct: standards of Conduct, Performance and Ethics. Nursing and Midwifery Council 2009.
An example of an effective training resource is ‘Confidentiality and young people: improving teenager’s uptake of sexual and other health advice’. This publication is endorsed by the Royal College of General Practitioners, the British Medical Association, the Royal College of Nursing and the Medical Defence Union.
Deliberate breaches of confidentiality, other than as described below, should be serious disciplinary matters. Anyone discovering such breaches of confidentiality, however minor, including an inadvertent act, should directly inform a senior member of staff (e.g. the Caldicott Guardian) who should take appropriate action.
The duty of confidentiality is not, however, absolute. Where a health professional believes that there is a risk to the health, safety or welfare of a young person or others which is so serious as to outweigh the young person’s right to privacy, they should follow locally agreed child protection protocols, as outlined in Working Together to Safeguard Children. In these circumstances, the over-riding objective must be to safeguard the young person. If considering any disclosure of information to other agencies, including the police, staff should weigh up against the young person’s right to privacy the degree of current or likely harm, what any such disclosure is intended to achieve and what the potential benefits are to the young person’s well-being.
Any disclosure should be justifiable according to the particular facts of the case and legal advice should be sought in cases of doubt. Except in the most exceptional of circumstances, disclosure should only take place after consulting the young person and offering to support a voluntary disclosure.
Duty of Care
Doctors and other health professionals also have a duty of care, regardless of patient age.
A doctor or health professional is able to provide contraception, sexual and reproductive health advice and treatment, without parental knowledge or consent, to a young person aged under 16, provided that:
- She/he understands the advice provided and its implications;
- Her/his physical or mental health would otherwise be likely to suffer and so provision of advice or treatment is in their best interest.
However, even if a decision is taken not to provide treatment, the duty of confidentiality applies, unless there are exceptional circumstances as referred to above.
The personal beliefs of a practitioner should not prejudice the care offered to a young person. Any health professional that is not prepared to offer a confidential contraceptive service to young people must make alternative arrangements for them.
Copies can be obtained from Department of Health, PO Box 777, London SE1 6XH.
Good practice in providing contraception and sexual health to young people under 16
It is considered good practice for doctors and other health professionals to consider the following issues when providing advice or treatment to young people under 16 on contraception, sexual and reproductive health.
If a request for contraception is made, doctors and other health professionals should establish rapport and give a young person support and time to make an informed choice by discussing:
- The emotional and physical implications of sexual activity, including the risks of pregnancy and sexually transmitted infections;
- Whether the relationship is mutually agreed and whether there may be coercion or abuse;
- The benefits of informing their GP and the case for discussion with a parent or carer. Any refusal should be respected. In the case of abortion, where the young woman is competent to consent but cannot be persuaded to involve a parent, every effort should be made to help them find another adult to provide support, for example another family member or specialist youth worker;
- Any additional counselling or support needs.
Sexual Offences Act 2003
The Sexual Offences Act 2003 does not affect the ability of health professionals and others working with young people to provide confidential advice or treatment on contraception, sexual and reproductive health to young people under 16.
The Act states that, a person is not guilty of aiding, abetting or counselling a sexual offence against a child where they are acting for the purpose of:
- Protecting a child from pregnancy or sexually transmitted infection;
- Protecting the physical safety of a child;
- Promoting child’s emotional well-being by the giving of advice.
In all cases, the person must not be causing or encouraging the commission of an offence or a child’s participation in it. Nor must the person be acting for the purpose of obtaining sexual gratification.
This exception, in statute, covers not only health professionals, but anyone who acts to protect a child, for example teachers, Connexions personal advisers, youth workers, social care practitioners and parents.
Working Together 2018
Children and young people who are sexually exploited are the victims of child sexual abuse, and their needs require careful assessment. They are likely to be in need of welfare services and – in many cases – protection under the Children Act 1989. This group may include children who have been sexually abused through the misuse of technology, coerced into sexual activity by criminal gangs or the victims of trafficking. Every Local Safeguarding Children Board (LSCB) should assume that sexual exploitation occurs within its area unless there is clear evidence to the contrary, and should put in place systems to monitor prevalence and responses. The Department for Education published updated guidance in 2017 on Child Sexual Exploitation: Definition and Guide for Practitioners
Appendix 3: Safeguarding Children Board Risk Assessment Tool
Click here to view Appendix 3: Safeguarding Children Board Risk Assessment Tool
Appendix 4 Guidelines for Completion of Risk Assessment for Sexually Active Under 16’s
| Confidentiality/potential information sharing | You should explain to children and young people at the onset, openly and honestly, what and how information will, or could be shared and why, and seek their agreement. The exception to this is where to do so would put that child/young person or others at increased risk of Significant Harm. |
| Sexually active? | Have they ever had intercourse in the past or at present? If yes: refer to Fraser guidelines and continue If no: continue risk assessment and give appropriate advice and support. Discuss link to cervical cancer, having multiple partners and possible abuse if appropriate. If not already discussed (when referring to Fraser Guidelines) use this opportunity to inform young person of their rights and responsibilities, such as legalities of sex under 13 and 16 and unprotected sexual intercourse. |
| Likely to begin? | How likely is the young person to become sexually active in the very near future? Discuss if activity is being planned. If young person tells you they are likely to have sex give appropriate advice and support (e.g. condom usage). |
| Last sexual activity | This will determine the need for emergency contraception or pregnancy test. The young person may not be aware of the risks. |
| Last monthly period | Discuss risk of pregnancy, irregular periods etc. |
| Contraception used | Any contraception that has been used in the past. This will determine risk of Sexually Transmitted Infections (STI) and suitability for that young person. |
| STI risk | Importance of condom use, statistics on STI’s. Discuss all aspects of risk, diagnosis, treatment and contact tracing if appropriate. |
| Details of partner | Obtain name and age if possible. Refer to risk factors if the relationship causes concern. |
Appendix 5: Useful Telephone Numbers
Children’s Social Care (Referral and Assessment) |
Cambridgeshire Children Social Care – Tel: 0345 045 5203 Peterborough Children Social Care – Tel: 01733 864180 Emergency Duty Team (out of hours) – Tel: 01733 234724 |
Police |
Tel: 101 or 999 if immediate protection required |
Cambridgeshire and Peterborough NHS Foundation Trust |
Tel: 0300 555 5870 Single point of contact for all CPFT safeguarding communications: safeguardingthinkfamily@cpft.nhs.uk |
Sexual Assault and Referral Centre (SARC) The Elms: |
0800 193 5434 www.theelmssarc.org |
Cambridgeshire Community Services NHS Trust: |
Duty Phone: 01480 425386 Generic Mailbox: ccs-tr.childprotection@nhs.net CCS Children in Care/Looked After Children Service: ccs.cambs.chic@nhs.net |
North West Anglia Hospitals NHS Foundation Trust |
Safeguarding Children: Nwangliaft.childsafeguardingadm@nhs.net Midwifery: nwangliaft.maternitysafeguardingteam@nhs.net |
Cambridge University Hospital NHS Foundation Trust |
Generic Mailbox: add-tr.addenbrookes-safeguarding@nhs.net |
Clinical Commissioning Group |
Safeguarding Children: CAPCCG.safeguardingchildren@nhs.net |
Appendix 6: Consent – Cup of Tea
Consent. It’s a powerful word that, for some bizarre reason, is still argued about to this day. It seems many people still don’t really get what “consent” means.
As Rockstar Dinosaur Pirate Princess points out, it’s actually a pretty simple concept: “Whoever you are initiating sexy times with, just make sure they are actually genuinely up for it. That’s it. It’s not hard. Really”. And it shouldn’t be.
But for many, it still is. Mystifying, right? So RDPP broke it down in the best way possible: with a metaphor so simple, even those who have historically had trouble grasping the concept should be able to understand it. We’ll let her do the talking: If you’re still struggling, just imagine instead of initiating sex, you’re making them a cup of tea.
You say, “Hey, would you like a cup of tea?” and they go, “OMG, yes, I would LOVE a cup of tea! Thank you!” Then you know they want a cup of tea.
If they are unconscious, don’t make them tea. Unconscious people can’t answer the question, “Do you want tea?” because they are unconscious.
If you say, “Hey, would you like a cup of tea?” and they um and ahh and say, “I’m not really sure…” then you can make them a cup of tea or not, but be aware that they might not drink it, and if they don’t drink it then — this is the important bit — don’t make them drink it. You can’t blame them for you going to the effort of making the tea on the off chance they wanted it; you just have to deal with them not drinking it. Just because you made it doesn’t mean you are entitled to watch them drink it. If they say, “No, thank you,” then don’t make them tea. At all. Don’t make them tea, don’t make them drink tea, don’t get annoyed at them for not wanting tea. They just don’t want tea, okay?
They might say, “Yes, please, that’s kind of you,” and then when the tea arrives they actually don’t want the tea at all. Sure, that’s kind of annoying as you’ve gone to the effort of making the tea, but they remain under no obligation to drink the tea. They did want tea, now they don’t. Sometimes people change their mind in the time it takes to boil that kettle, brew the tea and add the milk. And it’s okay for people to change their mind, and you are still not entitled to watch them drink it even though you went to the trouble of making it.
If they are unconscious, don’t make them tea. Unconscious people don’t want tea and can’t answer the question, “Do you want tea?” because they are unconscious.
End
